My original intent was to look at the problem of what happens to a group of physicians who are sailing along with very high patient satisfaction ratings. Then for no particular reason, their ratings drop by about 20-25%. At the high point they did not question the validity of the ratings. They just assumed the satisfaction ratings reflected their high quality work. The problem is that nothing they did changed and suddenly their ratings were significantly lower and people were looking for explanations. Hence the title of this post. If these ratings really mean something in the first place the physicians are suddenly thrown into a lot of self doubt. If they believe the ratings are unscientific, designed by people who don't know much about survey design or sampling, and are actually biased because of the way the staff presents the surveys - they are much less worried.
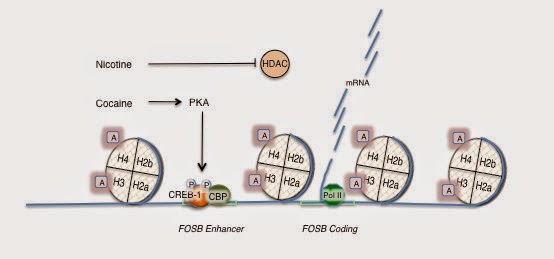
I posted to above bar graph as an introduction to this post. It is a composite of the opinions that several primary care physicians have given me about the correlation between benzodiazepine and opiate prescriptions and customer satisfaction ratings. More prescriptions for controlled substances equals greater customer satisfaction. Some clinics have adapted to this by letting patients know that they do not prescribe benzodiazepines or deal with psychiatric disorders. That eliminates physician-to-physician variability in prescribing. It also demonstrates that certain overprescribed medications are viewed as more serious than others. I have not for example seen any similar clinic rules for antibiotics even though they are also widely over prescribed.
I hope it is not a news flash to anyone that highly satisfied customers in the health care system have the highest mortality and probability of hospitalization (1). I know that at least some of the customers out there may be very surprised to hear that doctors can't be rated like a Toyota dealership. Toyota dealers after all have a product that is high in quality, uniform, and the same irrespective of those pesky human factors that we all have to deal with in human encounters. I am referring of course to things like communication, interpersonal skills, thinking capacity, personality traits and personality disorders. A Toyota dealer is out to satisfy all customer needs in the very circumscribed area of personal transportation. Even then there will be bumps in the road. A customer may not like the way the vehicle has turned out or some of the results from the service department. But generally Toyota dealers have a great product and most of their customers are highly satisfied.
This may be hard to believe but the MBAs that currently run medicine in the USA decided to introduce management principles into the field that were designed for the auto industry. The details and names of those management principles is irrelevant at this time, but when they were introduced it was a big deal. I had to listen to several hours of lectures on Six Sigma. Feel free to read about it and let me know how it possibly applies to the practice of medicine. After those lectures it was obvious to me that the MBAs running medicine were completely clueless about medical care. One small piece of evidence in what is now a mountain of evidence that the business emphasis in managing hospitals and doctors is completely off the rails. Most business concepts are introduced to groups of physicians as a manipulation. They have to be because no rational person would buy what appears to be Dilbert style management. It goes something like this:
"Look - we know that physicians don't like the idea that they can measured. We know you don't like that idea, but let's face it, this is a new era. Things aren't like they used to be. The day of the physician running things is over. You are all going to have to be accountable now. Some day your reimbursement is going to be tied to these satisfaction ratings."
Administrators like to seethe a little bit when they play the authoritarian act with physicians. They think it gives them more credibility. They could also be playing off the collective seething in the room. The logical questions followed:
"Well what about clinicians seeing patients with cognitive impairment or who are being treated on an involuntary basis. What can you say about the validity of those satisfaction ratings?"
That led to some laughter, but no explanations. Everybody would be rated and that was the end of it. There would be no exceptions. The irrational authoritarian business model rules.
Before anyone gets too bent out of shape about my view of the business model let me illustrate with an second example of what I mean. Earlier this evening I consulted with a colleague from another state on an inpatient problem. When that was over I asked her how things were going in general and she told me: "It's really kind of tough. The patients are never really stable, they have multiple psychiatric, substance use, and medical diagnoses and they are very hard to stabilize." She was thinking about moving on. She was in a meeting and an administrator said: "This patient has been here (x number of days) what is the plan?" She said: "What do you mean what is the plan? The plan is what the plan always is - stabilize the patient and discharge them." Managed care administrators have the uncanny ability to blame the physician for any discrepancy with a pure business approach to medicine. They apparently believe that hospital treatment and discharges are as predictable as Toyotas rolling off an assembly line. That is as true for customer satisfaction ratings as length of stay outliers. It give the administrators leverage against physicians, especially any physician who buys in to the idea that these are valid metrics.
Let me illustrate by considering two different physicians Doc A and Doc B. Both are very competent psychiatrists, but for some reason Doc A consistently scores lower on customer satisfaction ratings than Doc B. From the research in this area, it may simply mean that Doc B gives his patients more of what they want than Doc A. My speculation is that personality is a big factor. A simple mismatch between extroverts and introverts can fuel a lot of dissatisfaction. The extroverts on both ends (doctor and patient) like to be engaged and they like the conversation to have no dead air. A doctor that is too reserved may be perceived as being disinterested or not giving them enough in the interaction. Some patients want special treatment and others just want confirmation of their perceptions of other doctors and in: "I was not really impressed with your colleague. What do you think of him?" Psychiatrists generally know better, especially psychiatrists who recognize that their organization is set up to facilitate splitting and chaos. There may be a difference between the doctors in terms of prescribing patterns in terms of my previous analysis of the overprescribing problem. In this case Doc A may be known for no sleep medications, no benzodiazepine prescriptions, no opiate maintenance prescriptions and no high dose amphetamines for narcolepsy and no stimulant prescriptions for adult ADHD when the patient is functioning well in school or work. Denying those groups of prescriptions will not only result in low physician satisfaction scores but threats of violence and suicide. That is not to say that other tests or medication would not result in and extremely dissatisfied patient. There are thousands of scenarios where the patient does not take the physicians advice in the manner with which it is intended and that is - the best possible advice to diagnosis or treat a problem at a given point in time.
I did not write this post to "prove" that being satisfied with your physician is necessarily a good thing or a bad thing. If I wanted to approach problems like that I could probably get my own TV show. The whole point here is that any potential patient-customer needs to know what these things mean. You may not want to keep hearing the word but politics is the major reason. People trying to sell their business based idea about medicine versus physicians who have no similar notions. People trying to sell their idea that medicine is just like making widgets rather than treating people who have tremendous biological variability. You don't want your Toyota to have tremendous mechanical variability, but for human beings biological variability is both a fact of life and a distinct advantage from an evolutionary standpoint.
And finally what about news from your physician that you don't want to hear. Certainly there is widespread fear of a dreaded incurable diagnosis. There is the concern of diagnoses associated with disability and loss of function. But there is also straightforward advice on how to avoid fatal illnesses and disability. The way that is presented varies considerably from physician to physician. You have to ask yourself: "Would I rather hear that I am overweight and need to lose weight or that I should stop smoking or that I should stop using hydrocodone or alprazolam or would I rather be talking with a physician who would keep quiet on those issues?"
I don't think there is a good study of the issue and if somebody knows one please let me know so that I can post it here. I can provide another anecdote. I worked with a group of women once many of who consulted a female internist who was bright, attractive and wore very high fashion clothing (their characterization not mine). Things were generally going along pretty well until this internist told some of them that they were overweight and needed to lose weight. That elicited a very strong reaction and it seemed amplified by their perception of this physician as being "perfect". When I thought about my experience with physicians - nobody has ever told me to lose weight even in situations where they should have. I suggested it to a physician once and he said: "I concur with your recommendation doctor" but never told me that outright. Social and cultural factors all play a part in the patients perception of the physician and their satisfaction ratings.
It is a good idea to keep all of those factors in mind in attempting to interpret physician satisfaction ratings especially since most consumer web sites focus entirely on these measures.
George Dawson, MD, DFAPA
1: Fenton JJ, Jerant AF, Bertakis KD, Franks P. The Cost of Satisfaction: A National Study of Patient Satisfaction, Health Care Utilization, Expenditures, and Mortality. Arch Intern Med. 2012;172(5):405-411. doi:10.1001/archinternmed.2011.1662
From the reference:
"Patient requests have also been shown to have a powerful influence on physician prescribing behavior, and our findings suggest that patient satisfaction may be particularly strongly linked with prescription drug expenditures." (p. 408)
"While we do not believe that patient satisfaction should be disregarded, our data suggest that we do not fully understand what drives patient satisfaction as now measured or how these factors affect health care use and outcomes. Therapeutic responsibilities often require physicians to address topics that may challenge or disturb patients, including substance abuse, psychiatric comorbidity, nonadherence, and the risks of requested but discretionary tests or treatments. Relaxing patient satisfaction incentives may encourage physicians to prioritize the benefits of truthful therapeutic discourse, despite the risks of dissatisfying some patients." (p. 409)
Supplementary 1: If you are a primary care physician I am very interested in your thoughts about how patient satisfaction scores correlate with prescriptions for benzodiazepines, opioids, and stimulant medications as qualitatively depicted in the above bar graph.


.png)

.jpg)